间歇性低氧可降低血糖
糖尿病低氧可能导致自主神经功能失调。间歇性低氧(IH)是一种改善低氧适应的技术,在2型糖尿病患者可以改善心肺反射,并且最终改善血糖浓度。为了验证一个回合的间歇性低氧是否能够发起一个可能导致更好低氧适应的持久反应,来自奥地利因斯布鲁克大学医学部的Luciano Bernardi教授及其团队进行了一项研究,该研究发现一个回合的间歇性低氧诱导一个初步的低氧适应,伴随心肺反射的改善和血糖的降低。该研究结果在线发表在美国《糖尿病治疗》(Diabetes Care)杂志上。
该研究招募14例无自主神经并发症的2型糖尿病患者,在一个回合1小时间歇性低氧(呼吸含氧13%的混合气体6分钟,5次,每次间隔6分钟)前、结束时、结束后3小时和6小时测量血压、心率、血氧饱和度、化学感受器反射(低氧和高碳酸通气反应,通气阈值)和压力感受器反射的敏感性。这些测量值在受试者仅呼吸室内空气(单盲方案)的安慰治疗期间重复(至少间隔1周,随机顺序)。
该研究结果表明,间歇性低氧显著增加高碳酸通气反应,并降低通气阈值,以及增加血氧饱和度和血压,然而心率变异性和压力感受器反射敏感性增加没有意义。间歇性低氧后血糖显著下降。在安慰治疗期间除了血氧饱和度增加,没有观察到这些变化。一些影响在间歇性低氧后持续3小时,且一些甚至在间接性低氧后一直持续到6小时。
该研究发现,一个回合的间歇性低氧诱导一个初步的低氧适应,伴随心肺反射的改善和血糖的降低。2型糖尿病患者可以从完整的(>2周)间歇性低氧干预应用中潜在获益。
与血糖相关的拓展阅读:
- PNAS:胰高血糖素通过自分泌信号调节自身合成
- 良好的血糖和血压控制有益于延长糖尿病患者生存期
- ADA与ENDO低血糖共识
- Diabetes Care:良好的血糖和血压控制有益于延长糖尿病患者生存期
- Diabetes Care:ADA与ENDO低血糖共识 更多信息请点击:有关血糖更多资讯
Effects of a Single Bout of Interval Hypoxia on Cardiorespiratory Control and Blood Glucose in Patients With Type 2 Diabetes Mellitus
OBJECTIVE
Hypoxia may cause functional autonomic imbalance in diabetes. Intermittent hypoxia (IH), a technique improving the adaptation to hypoxia, might improve cardiorespiratory reflexes and, ultimately, blood glucose concentrations in patients with type 2 diabetes. We tested whether a single bout of IH could initiate a long-lasting response potentially leading to better adaptation to hypoxia.
RESEARCH DESIGN AND METHODS
In 14 patients with type 2 diabetes without autonomic complications, we measured blood pressure, heart rate, oxygen saturation, chemoreflex (hypoxic and hypercapnic ventilatory responses, ventilatory recruitment threshold), and baroreflex sensitivity before, immediately after, and 3 and 6 h after a 1-h single bout of IH (6-min breathing of 13% oxygen mixture 5 times each separated by 6-min recovery). The measurements were repeated on a placebo day (at least 1 week apart, in random sequence) when subjects were only breathing room air (single-blind protocol).
RESULTS
IH significantly increased hypercapnic ventilatory responses and reduced ventilatory recruitment threshold, and increased oxygen saturation and blood pressures, whereas increases in heart rate variability and baroreflex sensitivity were not significant. Blood glucose significantly decreased after IH. No such changes were observed during the placebo day, except an increase in oxygen saturation. Some of the effects lasted 3 h after IH, and some even persisted until 6 h after IH.
CONCLUSIONS
A single bout of IH induced an initial adaptation to hypoxia, with improvement in cardiorespiratory reflexes and reduction in blood glucose. Patients with type 2 diabetes could potentially benefit from the application of a full (>2 weeks) IH intervention.
影响因子:8.42
http://www.cmt.com.cn/subjectDetail/0/12/215495.html
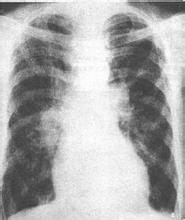
 此主题相关图片如下:1.jpg
此主题相关图片如下:1.jpg